Your Custom Text Here

Existing MTM Research
Thanks to Food Is Medicine Massachusetts (FIMMA) for this summary.
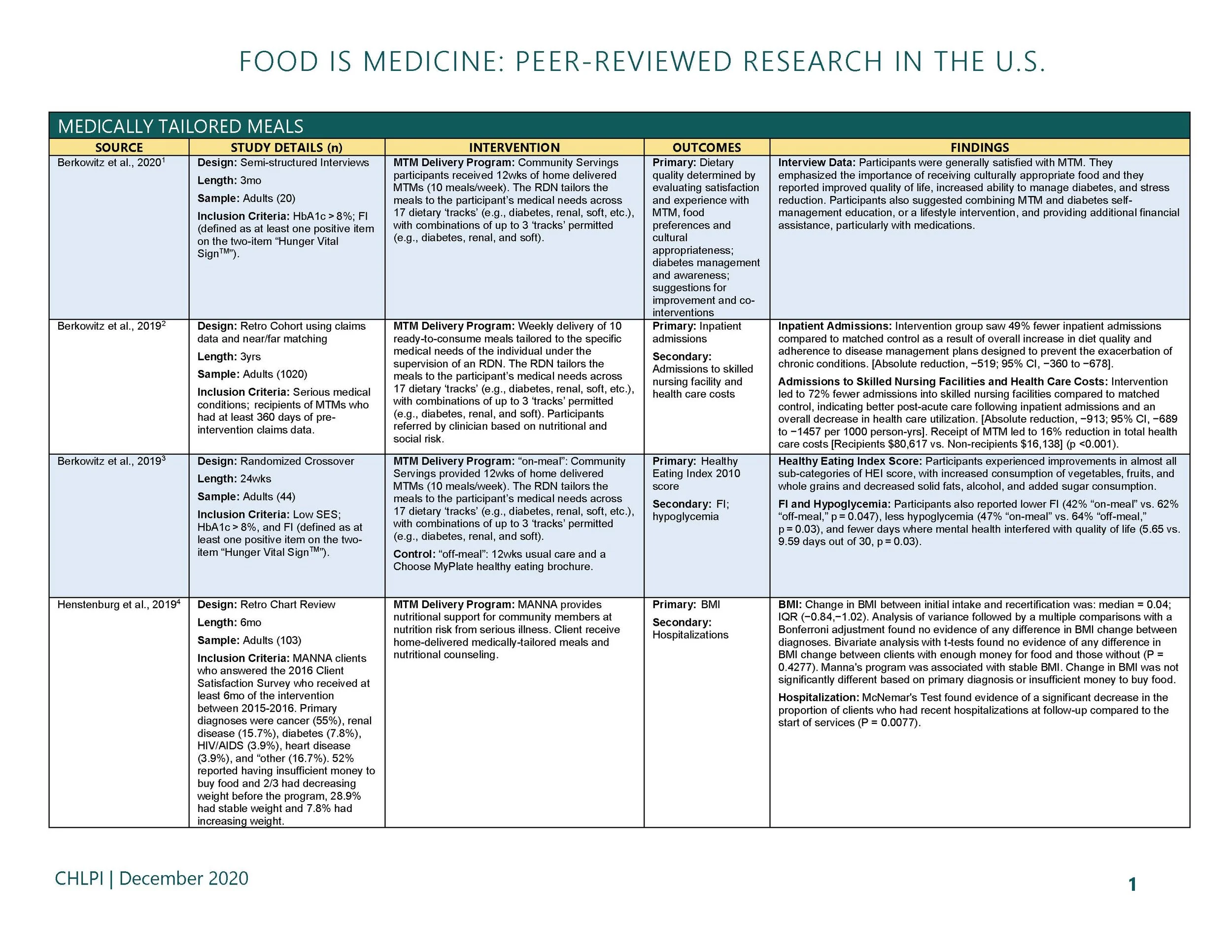
Receipt of MTM services (10 meals delivered weekly) was associated with significantly fewer inpatient admissions, (incidence rate ratio [IRR], 0.51; 95% CI, 0.22-0.80; risk difference, -519; 95% CI, -360 to -1457 per 1000 person-years).
Intervention receipt was associated with fewer skilled nursing facility admissions (IRR, 0.28; 95% CI, 0.01-0.60).
The model estimated that, had everyone in the matched cohort been encouraged into treatment (and including the cost of program participation), mean monthly costs would have been $3838 vs $4591 if no one had been encouraged into treatment (relative risk of mean per person per month expenditures difference, 0.84; 95% CI, 0.67-0.998; risk difference, -$753; 95% CI, -$1225 to -$280), representing approximately 16% lower health care costs.
In a randomized cross-over study, when participants with type 2 diabetes received medically tailored meals, they experienced substantially improved diet quality as measured by the 2010 USDA Healthy Eating Index (HEI).
The average HEI score (out of 100 possible points, with 100 representing the healthiest diet) for participants on medically tailored meals was 73.1, in comparison the average HEI score without medically tailored meals was 39.9 (p<.0001).
While receiving medically tailored meals, participants also reported lower food insecurity (42% "on-meal" vs. 62% "off-meal”), less hypoglycemia (47% "on-meal" vs. 64% "off-meal") and fewer days where mental health interfered with quality of life (5.65 vs. 9.59 days out of 30) (all p<.05).
Individuals dually eligible for Medicare and Medicaid who received medically tailored meals from Massachusetts-based Community Servings for 6 months had 50% fewer inpatient admissions and 70% fewer emergency department visits than similar patients not enrolled in the meal program (p<.05).
Researchers found an average net savings of $220 per patient per month (16% savings on total medical expenditures) after factoring in the costs of the medically tailored meals.
Adherence to antiretroviral therapy for HIV patients increased from 47% at baseline to 70% (p = 0.046) at the end of the 6-month intervention.
Diabetes distress (p < 0.001) and perceived diabetes self-management (p = 0.007) improved for patients with type 2 diabetes after 6 months of medically tailored meals.
The study observed decreased depressive symptoms (p = 0.028) and decreased binge drinking (p = 0.008) at the end of the intervention for all diagnoses.
Fewer participants sacrificed food for health care (p = 0.007) or prescriptions (p = 0.046), or sacrificed health care for food (p = 0.029) once they were connected to medically tailored meals.
The total average monthly health care costs for recipients of medically tailored meals were 31% lower than the comparison group ($28,000 vs.$41,000) at the end of the three-month intervention (p=.0006).
93% of the treatment group with inpatient hospitalizations were discharged to their homes as compared to only 18% of the comparison group (p=.0001).
From the Center for Health Law and Policy Innovation at Harvard Law School